A major gap in burn care is the lack of safe and effective topical or systemic agents that reduce burn progression and scarring. Burn injuries progress over time as a result of an intense inflammatory response and oxidative stress. Curcumin is a non-toxic spice with anti-inflammatory and anti-oxidant activities that has been used to treat non-burn wounds for hundreds of years. Recently, the Singer laboratory (Stony Brook University) found that pretreatment of pigs with oral curcumin reduced the extension of the ischemic zone in burns and improved healing (Figure 1).
Contact burn model (image A) results in several full-thickness burns separated by narrow uninjured interspaces representing the zone of ischemia (image B). In untreated wounds (control comb burn – image C) conversion of all three interspaces to full necrosis 1 week after injury was measured. In contrast, Image D shows that oral curcumin treatment reduces the percentage of unburned, ischemic interspaces that progress to necrosis. One indicator of cutaneous viability in the interspaces is the growing hairshafts (arrows in image D) that are beginning to cover the dark burn eschar. However, several inherent barriers are limiting the clinical use of curcumin, including bioavailability in both humans and animals due to its poor absorption, rapid metabolism and systemic elimination.
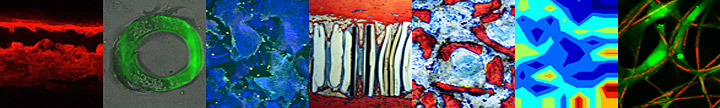
Figure 1. The effects of oral curcumin on the healing of burns examined using the contact thermal injury model in pigs
|
|
Larisa Sheihet, PhD measuring
the size of curcumin-loaded nanospheres using Dynamic Light Spectroscopy (DLS)
|
The Kohn Lab developed tyrosine-derived nanospheres that act as an effective sink for binding lipophilic drugs. In fact, curcumin complexation with these nanospheres resulted in its enhanced stability (Figure 2) in aqueous environment and topical delivery to cadaver skin. Skin permeation of curcumin-loaded nanospheres efficacy was compared to a pharmaceutically accepted drug solubilizer and carrier propylene glycol (PG) (Figure 3). Qualitatively and quantatively nanospheres clearly promoted penetration of curcumin into deeper layers of skin as compared to propylene glycol. Curcumin penetration into both superficial and lower dermis is about 30% higher when applied in nanosphere formulation. Therefore, the focus of this research will be to better understand curcumin mechanism of action in burn treatment, further optimize its topical delivery via tyrosine-derived nanospheres, and ultimately test curcumin-loaded nanospheres in validated animal models.

|
|
 |
Figure 2. Curcumin stability over a period of 24 hours as a function of the dispersion media. Tyrosine-derived nanospheres substantially enhance (6 fold) the stability and (180 times) aqueous solubility of curcumin compared to physiological solution (PBS).
|
|
Figure 3. Cross-sectional images obtained following 24 hours of passive permeation of curcumin into human cadaver skin.
|
Project Leader: Larisa Sheihet, PhD
Funding Source: U.S. Army Medical Research and Materiel Command (USAMRMC), the U.S. Army Institute of Surgical Research (USAISR), the Office of Naval Research (ONR), and the National Institutes of Health (NIH). This award is supported by contract number W81XWH-08-2-0034, Armed Forces Institute of Regenerative Medicine.